Most healthcare organizations think they’re secure because they passed their HIPAA audit. That’s the problem.
HIPAA compliance is about meeting legal requirements it’s the baseline for protecting patient data and staying out of regulatory trouble. But here’s what compliance frameworks don’t do: they don’t defend you against actual cyber threats. They set minimum standards, not security strategies. And there’s a massive difference between those two things.
Healthcare breaches keep happening despite organizations maintaining compliance. The issue isn’t HIPAA itself. The issue is treating compliance like it’s the same thing as security.
Where Compliance Actually Ends
HIPAA’s Security Rule gives you broad guidelines. Conduct risk analyses. Implement access controls. Encrypt data in transit. These requirements are foundational, sure. But they’re not specific enough to defend against sophisticated attacks.
Think about what healthcare organizations deal with every day:
- Cloud environments running hundreds of different services with complex configurations. HIPAA says implement “technical safeguards.” OK, but which ones? How do you actually secure a multi-tenant cloud setup where your data sits next to someone else’s?
- Medical IoT devices everywhere infusion pumps, monitors, ventilators all connected to your network. Most are running software that can’t be patched without voiding warranties or breaking FDA compliance. HIPAA requires access controls, but that doesn’t solve the fundamental problem.
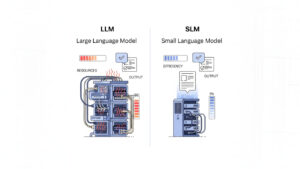
- AI systems processing clinical data. LLMs didn’t exist when the compliance checklist was written. Organizations are figuring out governance as they go.
- Ransomware attacks that are getting more targeted every month. Threat actors spend weeks mapping out healthcare environments before they strike. The standard compliance measures? They don’t prepare you for that.
HIPAA was written almost 20 years ago. It uses intentionally broad, technology neutral language. That made sense at the time. But it means the framework can’t keep pace with how fast threats and technologies are evolving.
What Real Security Actually Requires
Going beyond compliance means building active defense capabilities. Not the stuff that shows up on audit checklists actual security operations.
Periodic risk analyses become continuous vulnerability scanning with automated patch management. Plus, you need processes for handling zero-day exploits when they drop. Basic access controls turn into XDR platforms and behavioral analytics that can spot anomalies in real time. Network segmentation that actually contains breaches before they spread across your environment.
Standard encryption gets upgraded to quantum resistant protocols (yes, this matters sooner than most people think). You need properly secured API gateways and specialized controls for data intensive workloads like medical imaging. Business Associate Agreements get supplemented with Cloud Security Posture Management tools, immutable infrastructure, and container security that goes way beyond what vendor attestations promise.
The timing difference matters here. Compliance looks backward at what controls existed during the last audit period. Security looks forward at surviving attacks that haven’t been invented yet.

The Legacy System Problem
Healthcare runs on equipment that’s old. Medical imaging systems, laboratory analyzers, surgical equipment this stuff costs millions and lasts decades. A lot of it runs on operating systems that haven’t been supported in years.
HIPAA knows this exists. The rule requires risk analyses that document vulnerabilities in legacy systems. But compliance stops at documentation.
Security requires actual technical solutions. Network segmentation that isolates vulnerable systems. Intrusion detection tuned specifically to recognize attacks on legacy protocols. Compensating controls that take real expertise to implement correctly. This is where compliance and security diverge completely.
How to Actually Bridge the Gap
Organizations that get this right follow some common patterns.
- They use established security frameworks like NIST Cybersecurity Framework or HIMSS. These frameworks give you the technical depth and operational guidance that HIPAA’s requirements don’t cover. They’re not just more paperwork they’re operational playbooks.
- They bring in specialized expertise beyond regular IT roles. Medical device security, threat hunting, cloud security architecture these need different skill sets than general IT administration provides.
- They treat incident response as a core capability instead of an afterthought. That means response plans that get tested regularly and updated after every drill. Not documents that get created once to check a compliance box.
- They build security in from the start of every project. New applications, system upgrades, vendor integrations security can’t be retrofitted effectively. You either build it in or you’re accepting risk.

Moving Forward
HIPAA compliance stays necessary. Organizations have legal obligations and need to avoid penalties. But compliance by itself won’t stop breaches or protect patient data from the threats that actually exist right now.
The healthcare industry needs to rethink how it approaches security. Compliance gives you the legal foundation. Security gives you actual protection. They’re related but they’re fundamentally different objectives that require different investments.
Organizations that understand this distinction and invest accordingly? They’re in a much better position to defend against real threats.