INTRODUCTION
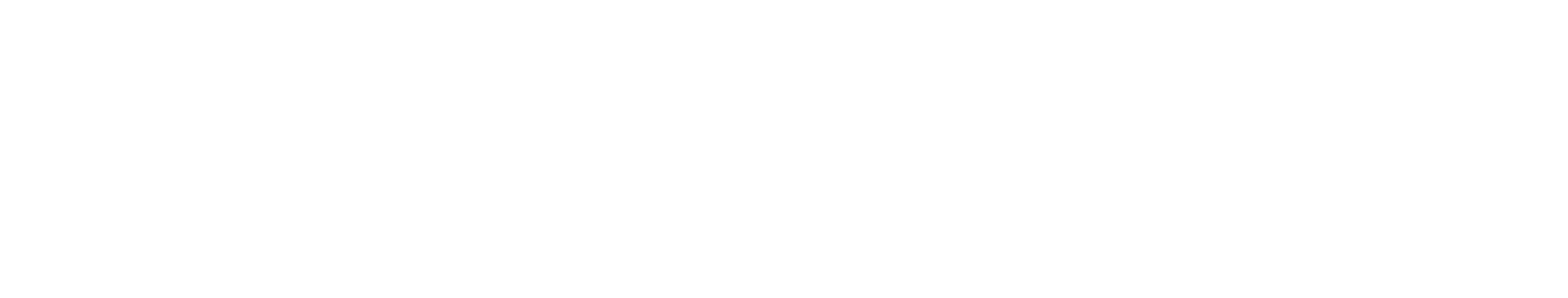
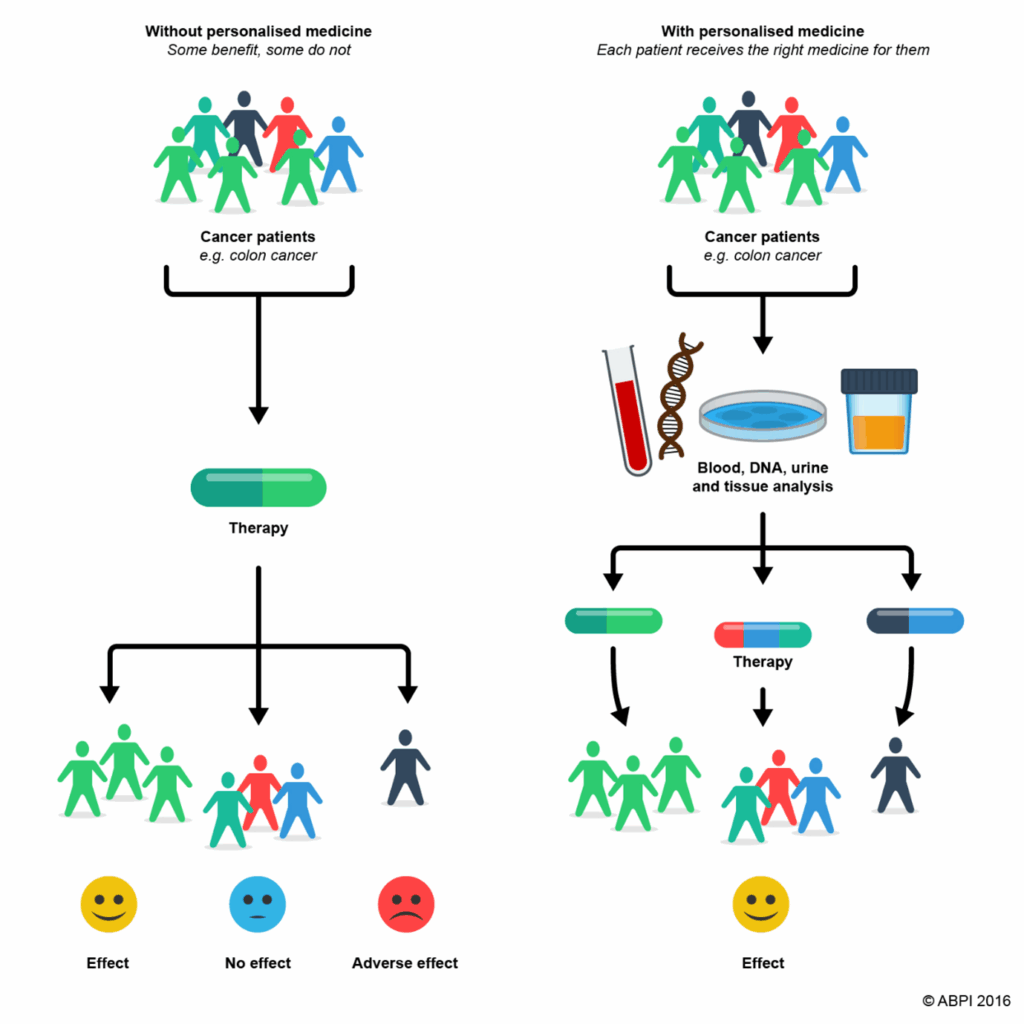
The reality that not every patient responds well to a particular treatment strategy is becoming more widely acknowledged in the medical community. Certain medical treatments and preventative measures may be effective for some individuals, but not for others. This understanding has led to a growing interest in personalised medicine, which aims to provide each patient the best care possible.
WHAT IS PERSONALISED MEDICINE?
The approach called “personalised medicine” analyses the distinctions among people with the same disease. It represents a shift away from the idea that “one size fits all.” According to this approach, certain patient groups ought to get the right care. Personalised medicine makes it easier to predict if a certain treatment will be beneficial for a particular patient. Despite its potential, personalised medicine must conquer a number of challenges before it can be widely incorporated into healthcare systems. Understanding that personalised medicine is an ongoing evolution in medical practice is crucial.
WHAT ARE THE BENEFITS OF PERSONALISED MEDICINE?
Personalised medicine has several benefits. By enabling more effective treatments and better patient outcomes through medications customised to an individual’s genetic profile, this method represents a substantial shift in healthcare. Both people and society at benefit from accurate diagnosis and focused therapy, which raise the possibility of therapeutic success and lower the risk of side effects.
The most significant application of personalised medicine has been in the treatment of cancer. For example, it is estimated that the United States is expected to diagnose over a million new cases of cancer annually. Tens of billions of dollars in lost productivity yearly are just one of the significant economic costs it imposes in addition to its impact on people. Through improved illness detection as well as customised preventive measures, Personalised Medicine has potential to reduce these impacts.
This is also true for infectious diseases like HIV, malaria, and tuberculosis, which are serious health problems in Africa and are thought to cost the continent more than $800 billion in lost output annually. To address these issues, the WHO has urged African countries to employ personalised medicine.
The preventive component of personalised medicine also enables more efficient use of resources by concentrating on specific disease pathways. This approach can reduce the need for long-term care and hospitalisation, enhance patients’ quality of life, and make treatments easier to manage.
Reducing the need for trial-and-error prescribing is another advantage of targeted treatments. Patients must try multiple medications before finding one that works because these approaches frequently fail due to genetic variations. This procedure can be significantly improved with a more personalised approach.
CHALLENGES OF PERSONALISED MEDICINES
Even while personalised medicine has several advantages in terms of diagnosis and treatment, there are substantial financial barriers. These treatments are often costly and can put a significant financial strain on patients, which limits accessibility. It is challenging for healthcare systems worldwide to integrate these unique medicines into regular medical services because to high development costs, intricate manufacturing procedures, and costly genetic testing and treatments.
Patients and the public may become concerned if personalised medicine raises health insurance costs. Maintaining patient access to these medications and controlling costs without restricting innovation are crucial. By doing this, we can guarantee that everyone has access to tailored treatment and lessen the financial strain on patients and healthcare systems. However, how can this be accomplished? As of right now, there isn’t a standard model. For instance, in several EU nations, the healthcare system doesn’t cover companion diagnostics, implying that patients are denied personalised medicine unless the drug manufacturer covers the cost of the diagnostic tests. This indicates these treatments are only beneficial for just a handful of individuals. Improving access to personalised medicine and promoting the sustainability of healthcare systems could be achieved by adjusting the cost of medications to match what people can afford in various nations.
Ethical and privacy issues are the other major barriers in personalised medicine. This is because personalised medicine utilises a lot of genetic and personal information, which may lead to concerns about safeguarding that data and ensuring that it is not misused. Therefore, it is important to keep this data from unauthorised users and to use it wisely. For personalised medicine to be successful, that is important. To solve this, experts are trying to find a healthy balance between preserving the privacy of individuals and providing researchers access to the data.
CONCLUSION
New personalised medicines are being approved, and the area of personalised medicine is expanding. These advancements have the potential to significantly alter healthcare. Many patients could benefit from better health outcomes because of personalised medicine’s potential to increase treatment efficacy and efficiency. Even though there currently exist many obstacles, with the right government assistance, personalised medicine might become a significant development in healthcare.